By Stefano Daniele DDS, MSc
The focus on prevention has reduced the incidence of caries in many western countries; however, we continue to observe a high rate of dental disease and decay. This is largely due to intrinsic conditions, such as gastro-esophageal reflux and gastric regurgitation (bulimia), and extrinsic dietary causes, such as continuous snacking, high sugar products, and soft-drinks that contain high levels of sugar and acids, which are known to cause aggressive enamel demineralization.1
A 46-year-old male was referred to my office with serious decay and hypersensitivity to cold. His patient history indicated he had undergone stomach constriction surgery to treat obesity. It also revealed a propensity for frequent consumption of a famous carbonated beverage with high erosive potential.2
The patient comes from a middle class socio-economic and cultural background. He is aware of the serious condition of his teeth, but he has no idea of the reasons for his condition. He reported to me that he brushes every day and is careful to practice good oral hygiene, even if he did not schedule regular visits to the dentist. It was only when he experienced hypersensitivity that he took a close look in the mirror and observed the clearly visible damage to his teeth. His major concerns were how this condition affected his smile and the impact of hypersensitivity on his quality of life. He was embarrassed by his teeth, and he could no longer tolerate cold food or drinks.
An initial examination showed large areas of demineralized enamel and exposed dentin, especially in the cervical area (Fig. 1). The extensive caries process could easily be traced to gastric regurgitation as consequence of stomach reduction surgery,3 and the frequent consumption of soft drinks.
I explained these causes and established the treatment plan. The patient was instructed to immediately modify his dietary habits and eliminate soft drinks; he was referred to a gastro-intestinal specialist to address the acid reflux episodes; he was instructed to rinse with sodium bicarbonate solution after each gastric regurgitation episode and avoid tooth-brushing after these episodes to prevent loss of demineralized and fragile superficial enamel;4 and he was placed on a fluoride-based mouthwash regime.
I restored the teeth using a mild self-etch adhesive and a conventional composite resin. However, at a 6-month recall visit, I noticed secondary caries at the restoration margins. Although improvements had been made in the patient’s diet and gastro-esophageal disorder, these had not been fully corrected.
Information on research and advances in dental materials are now readily available through journals, educational programs, and online portals. Through these sources I learned about an esthetic, bioactive, restorative material with a durable resin matrix (ACTIVA, Pulpdent Corporation, Watertown MA, USA). The material releases calcium, phosphate and fluoride ions5 that offer protection to the restorative-tooth interface, which is where secondary caries develops.
I removed the conventional composite restorations on the teeth affected by secondary caries, selectively etched the enamel, applied a self-etch bonding agent, and restored the teeth with ACTIVA (not shown).
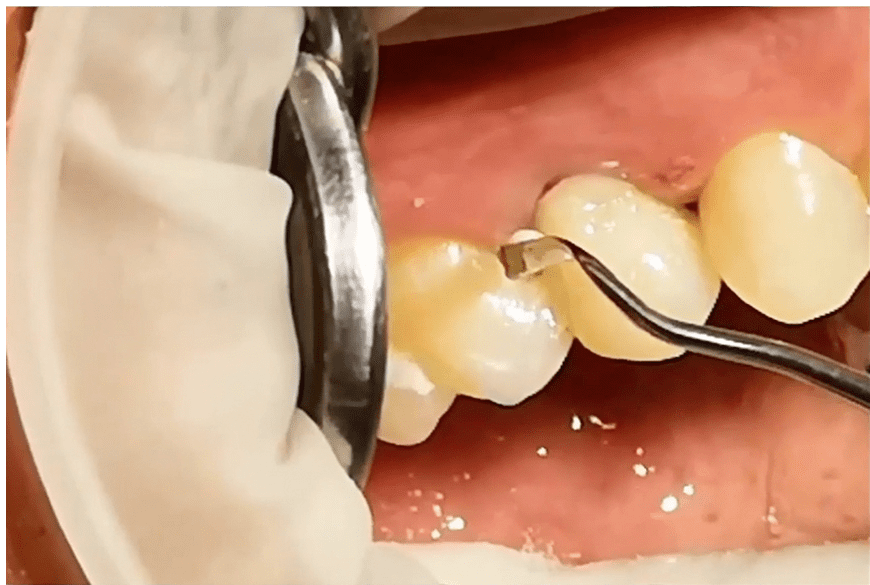
At this visit, I observed that a new active carious lesion had developed on the distal of the upper right lateral incisor (Fig. 2). This tooth had not been previously restored, and I treated this lesion with the bioactive material (Fig. 2-6).
The patient is still under my care, and the restorations placed with ACTIVA bioactive material did not show any staining or secondary caries at the one-year recall visit (Fig. 6).
The patient continues to show improvement. The gastro-esophageal regurgitation disorder has been reduced, and the patient follows the prescribed rinsing protocol after each episode. He has completely removed the erosive soft drink from his diet.
Patient history and patient education provide information to both the clinician and the patient that is essential for success. Lifestyle changes and medical interventions may be necessary to achieve desired outcomes. The restorative materials with bioactive properties could be a valid choice – and an alternative to the conventional procedures – in patients exposed to dental erosion, either of an intrinsic or extrinsic nature.







Specialist in restorative dentistry and endodontics
University of Milan, Italy
REFERENCE
1. Carvalho TS, Colon P, Ganss C, Huysmans MC, Lussi A, Schlueter N, Schmalz G, Shellis PR, Björg Tveit A, Wiegand A. Consensus report of the European Federation of Conservative Dentistry: erosive tooth wear-diagnosis and management. Swiss Dental Journal 2016:126; 342 – 346.
2. Kitasako Y, Sasaki Y, Takagaki T, Sadr A, Tagami J. Multifactorial logistic regression analysis of factors associated with the incidence of erosive tooth wear among adults at different ages in Tokyo. Clin Oral Investig 2017 Feb 7. doi: 10.1007/s00784-017-2065-7. [Epub ahead of print]
3. Barron RP, Carmichael RP, Marcon MA, Sandor GK. Dental erosion in gastroesophageal reflux disease. J Can Dent Assoc 2003;69:84-89.
4. Yip KH, Smales RJ, Kaidonis JA. Case report: management of tooth tissue loss from intrinsic acid erosion. Eur J Prosthodont Restor Dent 2003;11:101-106.
5. 45. Evaluation of pH, fluoride and calcium release for dental materials. Morrow BR, Brown J, Stewart CW, Garcia-Godoy F. J Dent Res 96 (Spec Iss A) 1359, 2017 (www.iadr.org).